
Ashton Leger
MSN, RN, Auburn University
AUSON MSN Curricular Outcome Mastery.
The mission of the School of Nursing is to foster and exemplify excellence in teaching, service/outreach, and research. The program prepares professional nurses to provide patient – centered, culturally competent, evidence based care for diverse populations in a dynamic health care environment. Master’s graduates are ready to lead in educator and advanced practice nurse roles in health-related services to diverse populations. Listed below are nine outcomes set by Auburn School of Nursing's MSN program. During the program, my education was based around these nine outcomes, both in the classroom and clinical arena. I have included examples, as well as documents, to prove I have met these outcomes and am ready to enter the field as a novice nurse educator and nurse practitioner.
1. Provide advocacy and leadership in the primary care setting that addresses the needs of culturally diverse populations, providers, and environments.
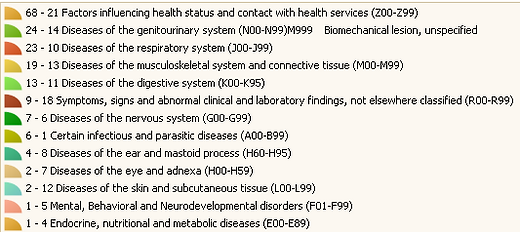
In March 2019 I had the invaluable opportunity to be a part of a medical mission trip to Quito, Ecuador. During this time, myself and 6 other NP students had the opportunity to practice independently as primary care, women’s health, and pediatric nurse practitioners. During the 4 day clinic we collectively saw and treated 395 patients, 71 of which I was responsible for. This experience opened my eyes to what practicing culturally competent healthcare truly means, as well as facilitators and barriers to performing it. We worked alongside undergraduate nursing students, pharmacy students, practicing NPs, a pharmacist, translators, and a physician from Quito. Acting as a leader and advocate in the NP role, I was able to ensure that my patients received the medications, referrals, testing, and care that they needed. Below you will see a graph of the ICD-10 codes for my patients seen in Ecuador. See the Ecuador tab at the top of this page as well for a glimpse into my clinical experiences while in Quito, Ecuador.
2. Manage available technology and/or information systems in the delivery of primary care.
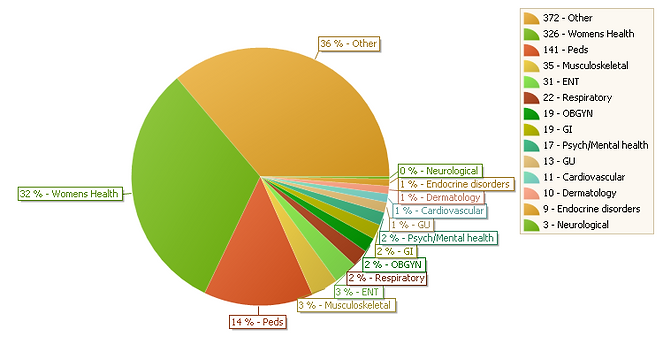
Technology is the future of medicine and can be seen throughout healthcare. Throughout my nursing career, as well as my MSN clinical rotations, I have worked with several electronic medical record systems such as: Cerner, Centricity, Athena, and Greenway. I have also been able to use many different computer programs throughout the MSN program such as Excel, Word, Powerpoint, Prezi, SPSS, and more. The MSN program utilized Medatrax, a system that allows students to keep track of patient encounters during clinical rotations. I completed more than 690 clinical hours, as well as 120 education practicum hours. You can see below a graph detailing the case types related to patients during my various clinical rotations.
3. Assume a position in a primary care setting as a primary care nurse practitioner, upon successful completion of national certification exam.
This e-portfolio documents my graduate experience and education. The courses that make up the curriculum at Auburn University's MSN Program have provided me with the knowledge needed to transition from a registered nurse to a nurse practitioner and nurse educator. Through rigorous coursework and 690 clinical hours, I have gained the knowledge needed to successfully obtain a master’s degree of nursing, pass the national certification exam, and acquire a position as both a nurse practitioner and nurse educator.
4. Utilize and conduct research that will promote quality health care and its delivery to improve clinical outcomes for selected population groups.
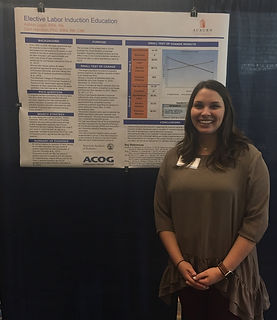
Three consecutive semesters in the MSN program were devoted to an EBP project. EBP is the use of current best evidence in making decisions about the care of individual patients. My project was aimed to reduce the number of elective labor inductions within one OBGYN practice in Dothan, Alabama. My small test of change (STOC) was to further evaluate the implementation of education regarding induction of labor and the effect it had on the mother’s decision whether to induce her labor or allow spontaneous labor to occur. Through my STOC, we saw the mean elective induction rate decrease from 60.4% before project implementation to 33.3% after induction education was introduced. The poster below summarizes this project including the significance of this project along with the results. I chose elective labor inductions because it is something I do every day at work, that is not always in the patient or neonate’s best interest. Nurse educators and nurse practitioners can educate both students and patients on this topic to help improve and promote better patient outcomes.
5. Establish a practice that includes lifelong learning, incorporation of professional standards, and mentorship with patients, families, and health care professionals.
A course titled “Roles and Issues of the Primary Care Nurse Practitioner” facilitated my exploration of the complex development for the APRN within the healthcare system. Advanced practice nursing has many roles in healthcare today, with one role being fulfilled by the NP. NPs are the largest group of advanced practice registered nurses (APRNs). The roles of an NP as related to an APRN include evidence and research-based practice, diagnostic reasoning to develop a plan of care, and patient care management. As APRNs, the NP provides continuous, comprehensive care throughout the lifespan in a diverse number of settings. Through assignments in this class, I was able to explore the role of the APRN and establish the way I will practice as an NP.
6. Provide comprehensive primary health care emphasizing health promotion and disease prevention to individuals, families, and groups across the lifespan.
Health Promotion and disease prevention is one of the most important aspects of caring for a population. Prevention leads to a better quality of life for patients and a decreased burden on the healthcare system. During my pediatric clinical rotation, I provided many children and their guardians with education regarding oral health. The education was delivered by a tri-fold pamphlet that the children could take home. The brochure consisted of background information on teeth, instructions of proper brushing, complications from inadequate care, and a diet to promote healthy choices to prevent further tooth decay.
7. Implement culturally competent primary care with a focus on quality improvement and safety that incorporates the socioeconomic, political, ethical, and diversity variable of each population.
Cultural competence necessary to provide quality care to a population. The MSN program devoted much time and effort in creating culturally competent nurse practitioners. I have had many learning opportunities, as well as experience caring for diverse populations including a multitude of races, religions, socioeconomic groups and ages. The graph below illustrates the diverse patient population I cared for during my clinical rotations. See the Ecuador tab at the top of this page as well for a glimpse into my clinical experiences while in Quito, Ecuador.

8. Apply theoretical foundations and change principles while leading in the development and implementation of innovations that advance practice in a primary care setting.
Nursing theories are the building blocks that lead to the development of all nursing concepts. The advance practice nurse utilizes various theories to understand and expand their nursing knowledge. Understanding different nursing theories allows an advanced practice nurse to practice in a more well-rounded manor, and in turn improve patient care. During our graduate theory class, I researched and wrote a concept analysis on learned helplessness.
9. Use ethical principles in decisions regarding issues related to individuals, populations, and health care delivery systems.
Health care providers are expected to act in the best interest of their patients. Unethical practices by health care providers can lead to unfavorable, and at times detrimental effects for their unsuspecting patients. Ethics is an imperative part of nursing education to instill decision making skills that protect the patients. My second semester included a class called Healthcare Policy and Ethics for Nurse Leaders. In this class we created an ethical case analysis. I conducted an ethical case analysis on the ethical dilemma of The Patient Protection and Affordable Care Act (PPACA). I found that the PPACA has created many ethical issues and challenges for government officials as well as healthcare providers.
10. Use appropriate teaching/learning principles to guide health teaching.
The course titled “The Professoriate” was invaluable, in that I learned an abundance of teaching strategies and games to use in my role as a nurse educator and nurse practitioner. Diversity is a topic nurses must not only consider in delivery of health care, but in nursing education as well. APRNs must acknowledge that differences in gender, socio-economic backgrounds, and culture all affect the learning environment. For example, individual differences of learners could potentially affect the learning style and learning readiness of the learner. APRNs must be cognizant of diversity, and willing to adapt to the needs of learners from various backgrounds. During my pediatric clinicals, I was able to apply these learned principles to my Oral Health teaching project and implementation.